This blog post is based on the points taken from TOG article Non-epithelial Ovarian Cancers published in July 2021. This article provides a detailed review to understand the classification, diagnosis and management of all NEOCs with focus on MOGCTs and SCSTs.
I hope you find this post helpful.
To access the original article : Click Here
To access all TOG topics : Click Here
 |
| https://www.rubabk4courses.com/courses/ |
Introduction
Ovarian Cancer in UK
• 6th commonest cancer in women
• Causes 4000 deaths per annum
Non-epithelial ovarian cancers NEOCs
• uncommon form of ovarian tumor
• 10% of all ovarian malignancies
• NEOCs can present at ANY age
• Classified into
• Malignant Ovarian Germ Cell Tumors - MOGCTs
• Sex Cord-Stromal Tumors - SCSTs
• Ovarian Sarcoma
• Small cell carcinoma of the ovary
Pathophysiology
• Ovaries divided into cortex and medulla
• Cortex made of ovarian follicles, interstitial gland cells & stroma
• Surrounded by dense capsule and surface covered with surface epithelium (coelomic)
• Epithelial ovarian tumors occur due to neomataplasia of surface epithelial cells
• SCSTs arise from different cell types from primitive sex cords and stromal cells
• Stromal cells include→ Theca cells, Fibroblasts & Leydig cells
• Primitive sex cords include→ Granulosa & Sertoli cells
• Germ cells arise from endodermal layer of the yolk sac
• Most non-epithelial ovarian tumors arise from these above specific cells (germ cells, granulosa cells, theca cells, stromal fibroblasts and steroid cells)
Clinical Presentation
• The commonest presenting symptoms — persistent abdominal distention, pelvic or abdominal pain, urinary urgency or frequency & menstrual irregularities
• In female of ANY age presenting with complex ovarian mass — must consider NEOC as differential diagnosis
Classification of Non-epithelial Ovarian Cancer
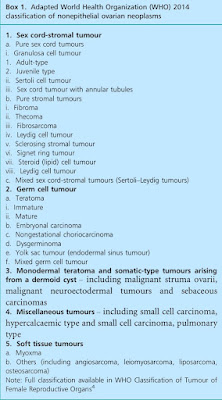 |
| Ref: TOG |
MOGCTs
• Usually occur in premenopausal women
• 80% of preadolescent ovarian malignancies
• Incidence 3.7 per 100 000 women per year
SCSTs can present at ANY age
• Adult-type granulosa cell tumors mainly in peri-menopausal & postmenopausal
• Sertoli-Leydig cell tumor occur in young
• Incidence 2.1 per 100 000 women per year
Malignant Germ Cell Tumors
Dysgerminomas — nests of polygonal cells with prominent nucleoli and clear glycogen-filled cytoplasm
Immature teratomas — elements from all 3 germ layers
Yolk sac tumors — microscopically large, with extensive areas of necrosis and hemorrhage; Schiller-Duval bodies is pathognomic
Sex Cord-Stromal Tumors
Granulosa cell tumors —large tumors with cystic/solid areas associated with mutations in FOXL2 gene
Sertoli-Leydig tumors — resemble embryonic testis & cause virilisation 22% have heterozygous elements (mucinous glands) 60% exhibit DICER1 mutation
Diagnosis and Tumor Markers
• TVS is the first line investigation for detecting malignancy
• CT used for staging
• MRI used when USG is inconclusive
• Serum CA125, Lactic Dehydrogenase (LDH), Alphafetoprotein (AFP) & Human Chorionic Gonadotropin (HCG) should be measured in ALL women <40 years presenting with complex ovarian masses
• CA125 to be checked in all postmenopausal
• Carcinoembryonic antigen (CEA) and CA19-9 can help in diagnosis of mucinous or endometrioid epithelial ovarian tumors or Krukenberg Tumors
• These are non-specific markers but their level correlates with staging and survival rates
 |
| Ref: TOG |
CA125
• Usually raised in epithelial ovarian cancers but only in 50% of early disease
• Can also be raised in endometriosis, fibroids and pelvic infections
• Not recommended for premenopausal women with simple ovarian cysts
• If taken level >200 U/ml to be discussed with gynaecological oncologist
• In postmenopausal RMI to be calculated
• Any score ≥200 CT abdomen & pelvis to be done
• Refer to MDT
SCSTs can present with hormone-mediated syndromes
Hyper-estrogenic SCSTs — may present with precocious puberty, abnormal uterine bleeding or endometrial hyperplasia
Hyper-androgenic SCSTs — may present with defiminisation, hirsutism, irregular menstruation, hoarse voice or male-pattern baldness
Inhibin B
• Expensive
• Not commonly used for diagnosis
• Part of follow-up protocols
Staging and Prognosis
 |
| Ref: TOG |
• FIGO staging is used for classification
• Full staging is done by surgical approach which includes omentectomy, biopsies of peritoneum and pelvic/para-aortic lymph nodes along with pelvic washings
• In suspected NEOC — fertility-sparing surgery should be initial approach in girls, adolescents and women wanting to preserve fertility.
• Pre-operative investigations include TVS; CT thorax, abdomen & pelvis; CXR and blood tests (including appropriate tumor marker)
• PET used in selected cases of germ cell tumors in case of inadequate surgical staging or for restating after adjuvant chemotherapy.
• Must perform endometrial curettage in women with granulosa cell tumors
• MOGCTs and SCSTs — highly sensitive to chemotherapy
• Can be successfully treated even in the advanced stage disease
• Over-all 5 year survival >80% (despite lung or lymph node metastasis)
 |
| Ref: TOG |
 |
| Ref: TOG |
Management
• Surgery & chemotherapy are cornerstones for treatment of NEOCs
• Aim of surgery — to remove all visible deposits
Fertility-conserving Surgery
• As NEOCs are common in young so unilateral salpingo-oophorectomy is a common practice
• Gold standard of management — full surgical staging
• Surgery often carried out through open route — midline laparotomy
• Laparoscopy may be useful in some cases—controversial (risk of spillage, inadequate staging and risk of port site metastasis)
• After surgery, the quantity of ovarian reserve is affected but successful pregnancies rates comparable to women with both ovaries intact
• Earlier menopause by one year in women with one ovary
Management of Malignant Germ Cell Tumors
• MGCTs 1.5% of ovarian cancers in EU 100 cases per year in UK
• 60-70% diagnosed in early stage & treated with surgery ± chemotherapy
• More sensitive to chemotherapy than SCSTs
• As most patients are young — more focus on fertility-sparing surgery along with chemotherapy
• Full staging can be associated with higher morbidity (if full lymphadenectomy done)
• More recently focus on lesser degree of surgical staging
 |
| Ref: TOG |
• Stage I cancer can be managed without chemotherapy Discuss with women the pros & cons of chemotherapy
• Relapse of stage 1a dysgerminoma 20% — most cured with salvage chemotherapy
Common adjuvant chemotherapy regimens
• Standard treatment regimen: 3-4 cycles of EP or BEP
• Etoposide & Cisplatin (EP) used in >40 yrs old
• Bleomycine, Etoposide and Cisplatin (BEP) used in <40 yrs old
• Side effects of BEP: ototoxicity & hearing loss, nephrotoxocity, pulmonary dysfunction, Raynaud’s phenomenon, avascular necrosis and secondary malignancies (especially Acute Myeloid Leukaemia)
• Risk of gonadal dysfunction leading to iatrogenic menopause & sterility — POF 3%
• Possible to have successful pregnancies after chemotherapy
Management of Sex Cord-Stromal Tumors
• 60-95% of all SCSTs diagnosed at early stage - Focus of treatment is surgery & chemotherapy
• Advanced stage— more extensive surgery & adjuvant chemotherapy
• SCSTs less chemo sensitive than MOGCTs
• Most with SCSTs are perimenopausal or postmenopausal
• Full staging surgery recommended (including hysterectomy + BSO)
• Fertility-sparing considered in individual bases
• Chemotherapy regimens — same like MOGCTs can also be treated with Carboplatin and Palitaxel
 |
| Ref: TOG |
Small Cell Carcinoma of Ovary- Hypercalcaemic Type (SCCOHT)
• Aggressive tumors Malignant Rhabdoid Tumors
• Associated with deleterious mutations of SMARCA4 remodeling genes
• Median age at presentation 24 years
• Serum calcium increased in 2/3 of patients
• Mostly unilateral
• 50% have extra ovarian spread @ diagnosis
• Chemosensitive but high risk of relapse
• No clear recommendations for management
• Cisplatin and Etoposide are agents of choice
• 5-year survival 10% -most die within 2 years of diagnosis
Ovarian Sarcoma
• Very rare
• Adenosarcoma & Carcinosarcoma - mixed epithelial and mesenchymal tumors (managed as epithelial ovarian cancers)
• Carcinosarcoma is the most common subtype
• Non-epithelial ovarian sarcoma — angiosarcoms, leiomyosarcoma, liposarcoma and osteosarcoma
• 80% occur in postmenopausal
• Median age @diagnosis 63 years
• Aggressive tumors & most present with distant disease
• Commonly spread to liver, lungs and retroperitoneal lymph nodes
• NICE recommends to manage in specialist sarcoma units which improves outcome MDT
• No clear consensus for treatment localized manage with surgery distant managed with chemotherapy (palliative)
• Agents used are Cisplatin, Doxorubicin, Ifosfamide
• Poor prognosis
Active Surveillance and Follow-up
 |
| Ref: TOG |
Germ Cell Tumors
• Recurrence of MOGCTs usually occur early
• Highest relapse in first 2 years
• Must follow active surveillance plan - 10 years
• Avoid pregnancy for first 2 years post-treatment
Sex Cord-Stromal Tumors
 |
| Ref: TOG |
• Standard follow-up regimens to be followed - history, examination (including pelvic), serum markers
• SCST relapse LATE
• Regular follow-up starts in 3rd year and continues indefinitely
• If lung metastasis suspected - CT chest abdomen & pelvis to be done
• All patients with fertility-sparing surgery to have 6 monthly pelvic USGs
Hormone Replacement
• In SCSTs → Avoid HRT
• In MOGCTs → Safe to use HRT & hormonal contraception
Psychological Support
• Early involvement of Teenage and Young Adult services
• Keep a holistic approach
Conclusion
· NEOCs are a broad group of malignancies
· Important to consider it as DD in young females with complex ovarian mass
· MDT involvement is essential
· Fertility-sparing surgery to be considered in those wishing to retain fertility
· Referral for oocyte preservation to be considered and discussed

Nice Dr Sb
ReplyDeletethanks
ReplyDelete