Sunday, December 26, 2021
Peripartum Cardiomyopathy
Wednesday, November 10, 2021
GTG 8 Amniocentesis and Chorionic Villous Sampling
This blog post is a Summary of Green Top Guideline 8: Amniocentesis and Chorionic Villous Sampling which was updated in October 2021. As it is a GTG so, it is must to go through the full guideline by yourself in order to have the complete understanding.
To download the guideline: Click Here
For Infographic: Click Here
For All GTGs: Click Here
 |
| RK4 Courses |
Background
- Prenatal diagnosis in the form on amniocentesis or CVS is offered due to various reasons such as higher risk for aneuploidy screening, suspected structural anomaly or in cases of known risk of inherited genetic disease
- The only definitive diagnostic tests → both CVS & amniocentesis
- CVS done between 11+0 - 13+6 wks Can also be done 14+0 - 14+6 wks
- Amniocentesis offered from 15+0 wks
- Individualised counselling
- Informed written consent Form 3
- Must provide information for aftercare
Organising amniocentesis & CVS
- Women are usually anxious so should support them ± partners
- Follow Fetal Anomaly Screening Program guidance
- Appropriate environment, skilled staff, access to allied specialities and appropriate support for continuation or termination of pregnancy
- Sensitive & unbiased approach
- Discuss religious aspects
- Give time to discuss the decision with partners & friends
Additional Risks with Invasive Testing
Risk of Miscarriage
- Additional risk of pregnancy loss after CVS or Amniocentesis is performed by an appropriately trained operator is < 0.5%
Different studies have been quoted
- Earlier studies showed increased pregnancy loss after CVS, but later studies show that there is no significant increase in pregnancy loss above the background risk with both procedures
- Lower pregnancy loss likely due to improvements in technology, techniques & experience
Systemic Review 2000-2014
- Procedure-related risk of pregnancy loss Amniocentesis 0.11% CVS 0.22% Both 0.35%
Cochrane Review comparing route for CVS (Transabdominal or Transcervical)
- Pregnancy loss below background rate regardless of route
- Procedure-related pregnancy loss Transcervical 1.4% Transabdominal 1%
Other risks
- CVS results may be affected by placental mosaicism in 1-2%
- Structural anomaly present → Discuss ongoing care (continuation or termination of pregnancy)
- Structural anomaly absent & QFPCR after CVS suggest chromosomal anomaly → full karyotype awaited before any decision
- Severe maternal sepsis → very rare
Saturday, October 09, 2021
Perinatal Mental Health -- Random Facts
This blogpost is a compilation of random facts about peripartum mental health which is one of an important aspect of women care. As a health care provider it is pertinent to provide optimum care for the mental health of the woman. Mental health disorders are prevalent and a woman is vulnerable during pregnancy and in the post part period. According to MBRRACE Suicide is now considered a direct cause of maternal death.
This post should be used as an adjunct to your study material for this topic as only random facts are given here.
I hope this is helpful for you all.
Thanks
 |
Psychiatric Disorders
- Common up to 20%
- 3-5% severely affected
- 2015 MBRRACE almost quarter of deaths due to this in 6wks - 1year postpartum
- Psychotic disorders more common than another time in a woman’s life
- Peak onset <7days
- Highest rate of adverse consequences of antenatal exposure Sodium Valproate
- Postpartum psychosis most commonly associated with bipolar affective disorder
- Approximate risk of developing postnatal depression with h/o depression + 1st degree family member with h/o postnatal depression 40%
The most common mental problems during pregnancy
- Depression 12% Anxiety 13%
- Both also affect 15-20% woman in the first year after birth
Psychiatric Assessment vital screening tool
Risks short term or long term
Red Flags Symptoms
- Rapid alteration in mental status
- New symptoms Psychotic symptoms
- Thoughts of violent self harm New ideas
- Guilt Hopelessness
- Acts of violent self harm
- Not eating well Insomnia
- Psychomotor retardation
Suicide risk found → trigger urgent assessment
- Local safe-guarding + infant protection issues
Screening Tools
- Wholly questions
- Edinburgh depression scale most frequently used
- Sensitivity 34-100% Specificity 44-100% PPV 57% NPV 99%
- PHQ-9 Patient Health Questionnaire 0-3
- GAD-2 & 7 Anxiety Screening tools
- Cut off scores — Mild 5 Moderate 10 Severe 15
- GAD -7 Sensitivity 89% Specificity 82%
- Moderately effective for panic disorders, social anxiety disorders, post traumatic stress disorders
Indications for Referral
- Current illness with symptoms of psychosis, severe anxiety, severe depression, sociality, self-neglect, harm to others or significant interference with daily functioning
- H/o bipolar disorder / Schizophrenia
- Hi/o serious postpartum mental illness like puerperal psychosis
Referral considered
- Illness of moderate severity
Monday, September 27, 2021
Non-epithelial Ovarian Cancers
This blog post is based on the points taken from TOG article Non-epithelial Ovarian Cancers published in July 2021. This article provides a detailed review to understand the classification, diagnosis and management of all NEOCs with focus on MOGCTs and SCSTs.
I hope you find this post helpful.
To access the original article : Click Here
To access all TOG topics : Click Here
 |
| https://www.rubabk4courses.com/courses/ |
Introduction
Ovarian Cancer in UK
• 6th commonest cancer in women
• Causes 4000 deaths per annum
Non-epithelial ovarian cancers NEOCs
• uncommon form of ovarian tumor
• 10% of all ovarian malignancies
• NEOCs can present at ANY age
• Classified into
• Malignant Ovarian Germ Cell Tumors - MOGCTs
• Sex Cord-Stromal Tumors - SCSTs
• Ovarian Sarcoma
• Small cell carcinoma of the ovary
Pathophysiology
• Ovaries divided into cortex and medulla
• Cortex made of ovarian follicles, interstitial gland cells & stroma
• Surrounded by dense capsule and surface covered with surface epithelium (coelomic)
• Epithelial ovarian tumors occur due to neomataplasia of surface epithelial cells
• SCSTs arise from different cell types from primitive sex cords and stromal cells
• Stromal cells include→ Theca cells, Fibroblasts & Leydig cells
• Primitive sex cords include→ Granulosa & Sertoli cells
• Germ cells arise from endodermal layer of the yolk sac
• Most non-epithelial ovarian tumors arise from these above specific cells (germ cells, granulosa cells, theca cells, stromal fibroblasts and steroid cells)
Clinical Presentation
• The commonest presenting symptoms — persistent abdominal distention, pelvic or abdominal pain, urinary urgency or frequency & menstrual irregularities
• In female of ANY age presenting with complex ovarian mass — must consider NEOC as differential diagnosis
Classification of Non-epithelial Ovarian Cancer
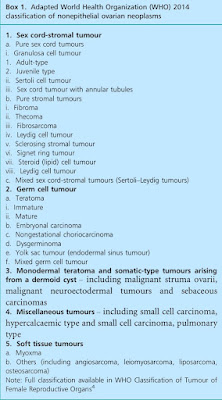 |
| Ref: TOG |
MOGCTs
• Usually occur in premenopausal women
• 80% of preadolescent ovarian malignancies
• Incidence 3.7 per 100 000 women per year
SCSTs can present at ANY age
• Adult-type granulosa cell tumors mainly in peri-menopausal & postmenopausal
• Sertoli-Leydig cell tumor occur in young
• Incidence 2.1 per 100 000 women per year
Malignant Germ Cell Tumors
Thursday, August 05, 2021
Surgical Site Infections in Obs & Gynae
The points in this post have been extracted from a TOG article published in April 2021. Surgical site infection poses a challenge for surgery and has huge impact on patient care/safety and healthcare system. It is an important cause of patient morbidity and if severe can even lead to death.
Different guidelines have been produced to address this issue. This article provides a very good resource of comprehensive information about SSI.
It is recommended to read the original article to grasp the topic completely.
I hope you find this post helpful.
Suggestions to improve future posts are welcome.
Thanks
 |
| https://www.rubabk4courses.com/courses/ |
Introduction
- SSI remains a peri-surgical problem
- May lead to severe morbidity & mortality, prolonged hospitalisation & enormous economic costs
Measure to reduce SSI
- Improved ventilation in OTs
- Equipment sterilisation
- Barrier use during surgery
Factors which increase SSI
- Antibiotic resistant pathogens, chronic disorders like DM, alcoholism, obesity & immunosuppression
- In obstetrics SSI associated with prolonged labour, emergency CS & multiple vaginal examinations
- Common pathogens include gram +ve & -ve organisms such as Staphylococcus aureus & E. Coli
Definition
- Infection of superficial or deep skin incision, or of an organ or space, occurring up to 30 days after surgery if no implant was left behind, or within 1 year if an implant was left in place
Specific Criteria for diagnosis
Superficial wound infection at least one of the following
- Purulent effluent or exudate with organisms identified
- One of following: pain, redness, localized swelling, tenderness or heat
- Diagnosis by surgeon or attending physician
Deep wound infection at least one of the following
- Purulent exudate from deep wound incision
- Spontaneous dehiscence of deep incisional wound or if deliberately opened with temp >30˚C, localized pain or tenderness
- Abscess or infection involving deep wound incisions
- Diagnosis by surgeon or attending physician
Organ or space infection at least one of the following
- Purulent exudate from a drain
- Organism isolated
- Evidence of abscess or infection
- Diagnosis by surgeon or attending physician
Wound Classification
 |
| Ref: TOG |
Epidemiology
- Incidence 2-6% of surgeries in high-income countries
- UK in 2006 survey
- Incidence of health care-acquired infection 8% out of which 14% were SSI
- 5% patients having surgery had SSI
- Incidence varies according to the type of surgery
- Highest after bowel surgery 8%
- Lowest after knee replacement 0.5%
- After TAH 1.6%
- After CS 3-15%
Risk factors
